Keratoconus is a complex, progressive condition. As with other eye diseases and disorders, increasing your understanding of what keratoconus is and the options available for treatment can be essential for knowing what to expect when it affects you or someone you know.
At a basic level of understanding, you may know keratoconus is a condition that can cause blurred vision, light sensitivity, and other symptoms and can be treated with corneal cross-linking, contact lenses and corneal transplants.
Each case of keratoconus can vary from person to person, and your options for cornea surgery and treatment may vary based on the progression of your symptoms and your individual eye health.
Understanding Keratoconus
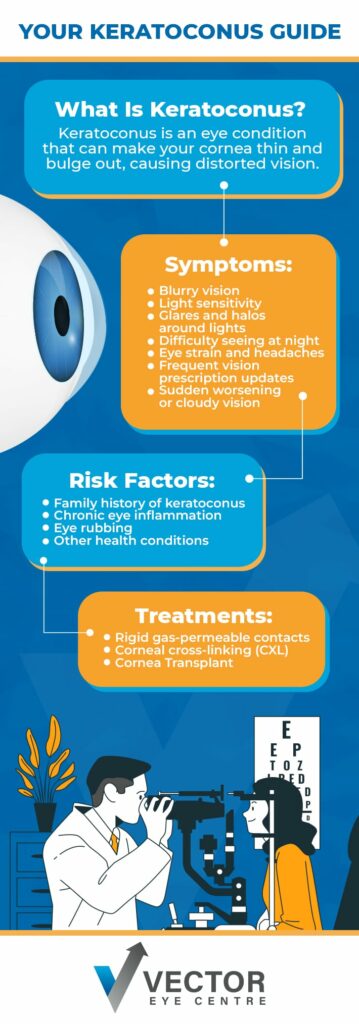
Keratoconus is a progressive condition that can cause your cornea—the clear, front part of your eye—to get thinner and change shape. As your cornea gradually thins, it can bulge out, causing distorted vision because of changes to how your eye focuses light.
At What Age Does Keratoconus Get Worse?
Typically, keratoconus first appears during the late teenage years, but it can also appear during a person’s 20s and 30s—so the exact age at which your symptoms appear or get noticeably worse may vary.
Because keratoconus is a progressive disease, it can continue to get worse over time. Getting an early keratoconus diagnosis through comprehensive eye exams during your teenage and young adult years is often vital for preserving your eye health.
What Are the Symptoms of Keratoconus?
Changes to the shape of your eye—or what may be referred to as an irregular curvature of the eye—can cause distorted vision because of the resulting changes to how light passes through your cornea and focuses on your retina.
When your cornea takes on a cone shape because of keratoconus, you may experience any of the following symptoms:
- Blurry vision
- Sensitivity to light
- Glares and halos around lights
- Difficulty seeing at night
- Eye strain and headaches
- Frequent vision prescription updates
- Sudden worsening or cloudy vision
It’s important to know that while these symptoms may be caused by keratoconus, they could also be caused by other eye diseases and disorders. Even dry eye disease can cause issues like light sensitivity and blurry vision.
If you’re experiencing any of the symptoms above, visiting an eye doctor and getting a clear diagnosis is crucial for moving forward with an appropriate treatment plan.
Can People with Keratoconus Go Blind?
Keratoconus does not cause blindness—but it can cause other serious changes to your vision that affect your daily life. Prompt treatment for conditions like keratoconus helps protect your sight and your long-term quality of life.
What Causes Keratoconus?
Unfortunately, the exact cause of keratoconus isn’t fully understood. If one or both of your parents have keratoconus, you may be more likely to develop it as well, which is one reason why keratoconus is sometimes referred to as a hereditary condition.
Other risk factors that can increase your chances of developing keratoconus include chronic eye inflammation and other conditions that can affect your overall health, such as Ehlers-Danlos syndromes, Down syndrome, and Marfan syndrome.
Are People Born with Keratoconus?
People are not born with keratoconus—it develops over time as people’s eyes change while they grow.
Changes to your eyes that occur over time–especially those that first appear during a person’s childhood and teenage years—are part of the reason why getting routine comprehensive eye exams is so important.
Does Rubbing Your Eyes Cause Keratoconus?
Keratoconus has been linked to chronic eye rubbing. Some studies have confirmed that eye rubbing can cause your cornea to thin out and lead to eye injuries that may cause keratoconus.
The exact effect of eye rubbing can vary, but if frequent eye rubbing is affecting you, your child, or another family member, you should consider visiting an eye doctor to find out what may be irritating your eyes.
How Is Keratoconus Treated?
The treatment we recommend for keratoconus may depend on the progression of your symptoms and your individual eye health.
During the early stages of keratoconus, you may be able to achieve clear vision with the use of standard eyeglasses or contact lenses, but eventually, keratoconus can progress to the point that using eyeglasses or soft contact lenses is no longer an effective or comfortable option for seeing clearly.
Contact Lenses
For moderate cases of keratoconus, rigid gas-permeable contact lenses (RGP lenses) may be recommended. The design of RGP lenses can create a fluid reservoir in front of your cornea that acts like a liquid lens, correcting the refractive errors caused by keratoconus and providing clear vision. However, there are many types of contact lenses that can be helpful depending on the shape and severity of the keratoconic cornea. Hybrid, piggyback and scleral contact lenses are all also contact lens types used to improve vision in keratoconus
Corneal Cross-Linking (CXL)
In some cases, we may recommend corneal cross-linking (CXL) as a treatment to help preserve your vision by stopping the progression of cornea thinning in keratoconus. CXL often can’t completely reverse the effects of keratoconus, but it can be helpful for protecting your remaining vision—and in some cases, it may improve your vision.
CXL involves applying a vitamin B solution to your eye and activating it with UV light to help new collagen bonds form and strengthen your cornea.
Corneal Transplants
For more severe cases of keratoconus, we may recommend other forms of cornea surgery, including a cornea transplant.
A cornea transplant involves replacing your existing cornea with new cornea tissue. Following the procedure, you may still need to wear eyeglasses or contact lenses to achieve full visual clarity.
If a cornea transplant is something that could benefit your eye health and lifestyle, we’ll take the time to discuss your options with you and answer your questions about what to expect before, during, and after the surgery.

When Should You See a Doctor for Keratoconus?
Whenever you notice changes to your vision or eye health, you should speak with an eye doctor. When you receive a diagnosis for keratoconus during an eye exam, we can work with you and your eye doctor to determine the right treatment plan for your needs.
We want to help you achieve clear, healthy sight and maintain your long-term eye health with modern treatments and a personalized approach to eye care.
Please contact us at Vector Eye Centre to learn more about keratoconus and the treatments we offer. We’re here to support your vision and quality of life.



