Keratoconus is a serious, progressive eye condition that affects the cornea. The good news is that blindness caused by keratoconus is extremely rare. However, without proper treatment and monitoring, this condition can lead to significant vision impairment that impacts your daily life and quality of vision.
Understanding keratoconus, its progression, and available treatment options can help you make informed decisions about protecting your eyesight.
What Is Keratoconus?
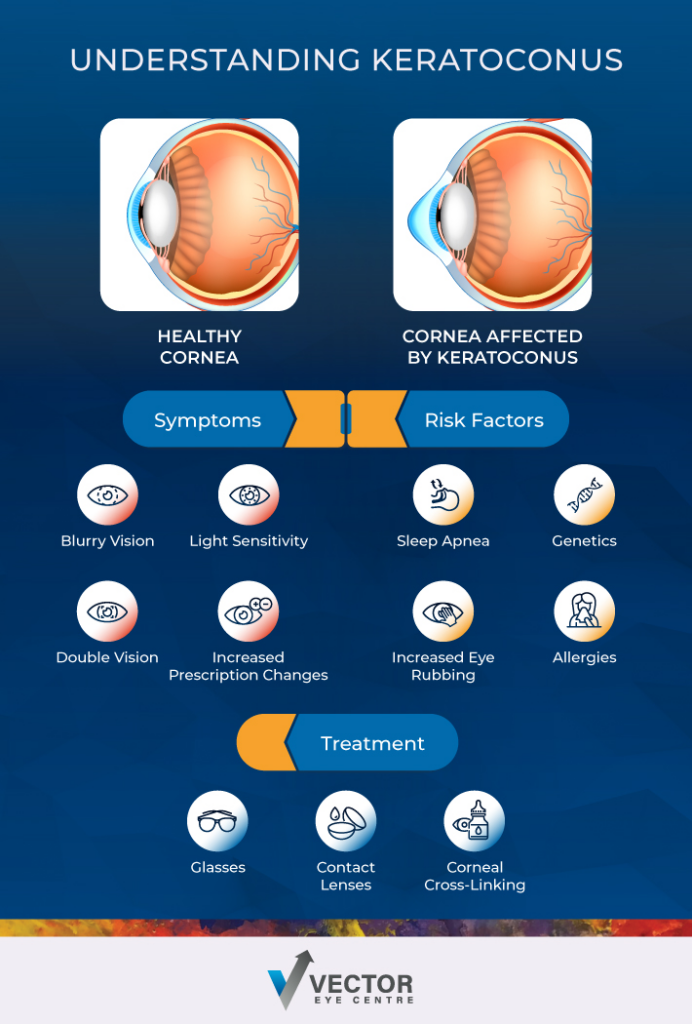
Keratoconus is a progressive eye disorder where the cornea—the clear, dome-shaped front surface of your eye—gradually thins and bulges outward into a cone shape. Typically, your cornea maintains a smooth, curved surface that helps focus light properly onto the retina. When keratoconus develops, this irregular shape distorts your vision and makes it difficult to see clearly.
The condition typically affects both eyes and may be asymmetric. Keratoconus most commonly begins during the teenage years or early twenties, though it can develop at any age.
Symptoms of Keratoconus
The early signs of keratoconus can be subtle and are often mistaken for normal vision changes. As the condition progresses, you may notice:
- Progressive, blurred or distorted vision that cannot be fully corrected with glasses
- Increased sensitivity to light and glare
- Frequent changes in eyeglass or contact lens prescriptions
- Double vision
- Difficulty with night vision
- Eye strain and headaches from trying to focus
- Seeing halos around lights
Risk Factors & Causes of Keratoconus
While the exact cause of keratoconus remains unclear, research has identified several risk factors:
- Genetics: A family history of keratoconus increases your risk
- Eye rubbing: Chronic, vigorous eye rubbing may contribute to corneal weakening
- Allergies: Conditions causing frequent eye rubbing, such as allergic conjunctivitis
- Connective tissue disorders: Conditions like Ehlers-Danlos syndrome
Understanding these risk factors can help you take preventive measures and seek early evaluation if you’re at higher risk.
How Does Keratoconus Progress?
Keratoconus progression varies significantly from person to person. Some people experience rapid changes over months, while others may have stable vision for years. Eye rubbing is a serious risk factor. Regular monitoring with your eye doctor helps track any changes and adjust treatment accordingly. The condition typically progresses through several stages:
- Mild stage: Slight corneal thinning with minimal vision changes that can often be corrected with glasses or soft contact lenses
- Moderate stage: More pronounced corneal irregularity requiring specialized contact lenses for clear vision
- Advanced and severe stages: Severe corneal thinning and scarring that may require surgical intervention
Can Keratoconus Be Treated?
Keratoconus cannot be cured, but numerous effective treatments can slow its progression, improve vision, and maintain your quality of life. Treatment approaches depend on the severity of your condition and how it’s affecting your daily activities.
Non-Surgical Treatment
- Eyeglasses: In mild cases, prescription glasses can provide adequate vision correction
- Contact lenses: Various specialized contact lenses, such as rigid gas-permeable lenses, hybrid lenses, and scleral lenses, offer excellent vision correction for keratoconus
- Corneal cross-linking: This minimally invasive procedure uses UV light and riboflavin drops to strengthen corneal tissue and slow progression
Surgical Treatment
When non-surgical options are insufficient, surgical interventions can restore functional vision:
- Intacs: Small plastic inserts placed in the cornea to flatten the cone shape and improve vision.
- Corneal transplant: In advanced cases, replacing the damaged cornea with healthy donor tissue may be necessary
Can Keratoconus Lead to Total Blindness?
The short answer is that total blindness from keratoconus alone is highly uncommon. But severe keratoconus can cause significant visual impairment that substantially impacts your ability to perform daily tasks.
In rare cases, complications such as corneal scarring, sudden corneal swelling, or corneal perforation can occur. Even in these severe situations, appropriate medical intervention can typically preserve some level of functional vision.
The key to preventing severe vision loss is early detection and proper treatment. With modern treatment options, most people with keratoconus maintain good functional vision throughout their lives.
What Happens If Keratoconus Goes Untreated?
Early intervention is always preferable and often leads to better long-term outcomes. Untreated keratoconus can lead to progressive vision deterioration.
Without proper management, you may experience:
- Increasing difficulty with daily activities like driving, reading, or working
- Frequent prescription changes that become less effective over time
- Development of corneal scarring
- Potential need for more invasive treatments later
Living with Keratoconus
A keratoconus diagnosis doesn’t mean the end of clear vision or an active lifestyle. Many of our patients at Vector Eye Centre continue to drive, work in demanding professions, and enjoy recreational activities with proper treatment and vision correction.
The key is working closely with your eye care team to find the right combination of treatments for your specific situation. Modern contact lens designs and surgical techniques offer excellent options for maintaining functional vision even in advanced cases.
Protect Your Vision with Vector Eye Centre
Keratoconus requires specialized care from experienced professionals who understand this complex condition. We’re proud to be one of the few clinics offering innovative surgical treatments for keratoconus.
Our comprehensive approach combines diagnostic technology with personalized treatment plans tailored to your specific needs. Whether you need specialized contact lens fitting, corneal cross-linking, or surgical intervention, our team has the expertise to help preserve and restore your vision.Contact our expert team today to schedule a comprehensive evaluation and learn about your treatment options.



