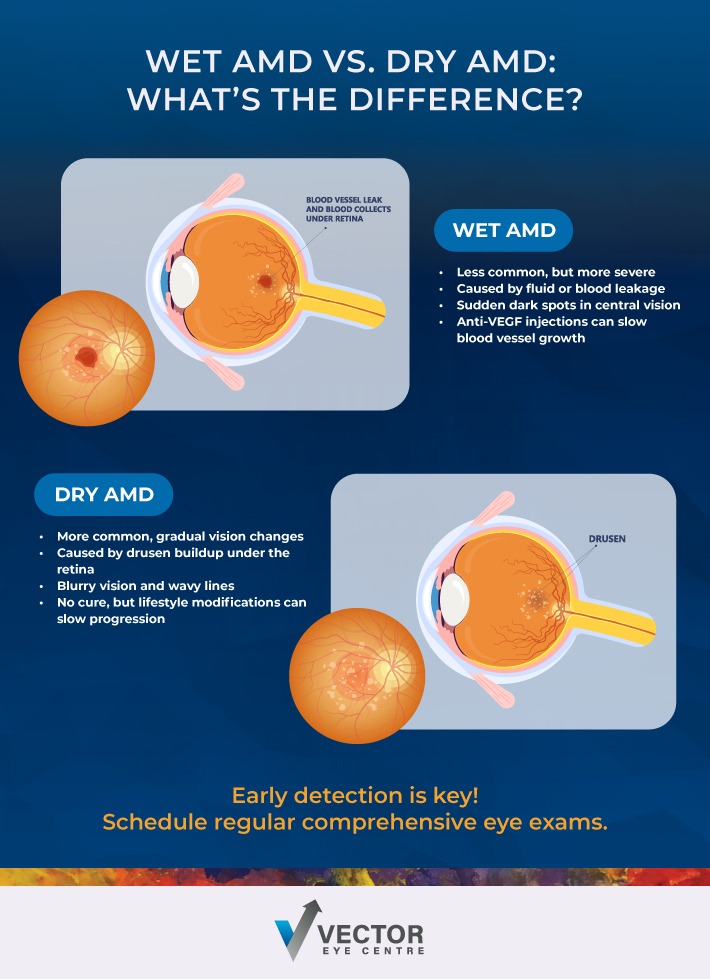
Wet and dry age-related macular degeneration (AMD) are 2 major forms of an eye disease that affect the macula. Dry AMD typically develops slowly and results in gradual vision loss, whereas wet AMD develops quickly and is often an emergency.
AMD affects many Canadians, making it one of the leading causes of vision loss in people over 50. While the prospect of developing AMD can feel overwhelming, understanding the condition—particularly the differences between its 2 main types—empowers you to take proactive steps toward preserving your vision.
What Is Macular Degeneration?
AMD is a primarily age-related eye disease that occurs when the macula—the small, central portion of your retina responsible for sharp, detailed vision—begins to deteriorate. This condition primarily affects your central vision, which you rely on for activities like reading, driving, recognizing faces, and seeing fine details.
The macula contains millions of light-sensing cells that work together to create the crisp, clear images you see when looking straight ahead. When AMD develops, these cells gradually break down, creating blind spots or distortions in your central field of vision. Fortunately, AMD typically doesn’t affect your peripheral vision, so complete blindness is rare.
Early Signs of AMD
Recognizing the early warning signs of AMD can make a significant difference in preserving your vision. Many people don’t notice symptoms in the initial stages, which is why regular eye exams are so important. However, as the condition progresses, you might experience:
- Straight lines appearing wavy or distorted
- Blurred, dark or empty spots in your central vision
- Difficulty seeing in low-light conditions
- Colours appearing less vibrant than usual
- Trouble recognizing faces or reading fine print
- Need for brighter light when reading or doing close work
Dry AMD
Dry AMD accounts for approximately 90% of all macular degeneration cases. This form of the condition develops gradually as small, yellow deposits called drusen accumulate beneath the retina. Over time, these drusen when present in a specific formation, number and size can cause the macula to thin and lose its structure, leading to vision changes.
Dry AMD typically progresses slowly, sometimes taking years or even decades to significantly impact your vision. The condition usually begins in one eye but often affects both eyes eventually. While dry AMD is less severe than its wet counterpart, it can still cause substantial vision loss over time and may progress to wet AMD at any time.
Wet AMD
Wet AMD is less common but more serious than dry AMD, affecting about 10% of people with macular degeneration. This form develops when abnormal blood vessels grow beneath the macula, leaking blood and fluid into the retinal tissue.
Unlike dry AMD, wet AMD can progress rapidly, sometimes causing significant vision loss within weeks or months. The transition from dry to wet AMD can happen suddenly, making regular monitoring crucial for anyone diagnosed with macular degeneration.
Key Differences Between Wet & Dry Macular Degeneration
Understanding the differences between wet and dry AMD helps you better navigate your condition and treatment options:
- Progression speed: Dry AMD often advances slowly over years, while wet AMD can cause rapid vision changes
- Prevalence: Dry AMD is much more common, affecting the vast majority of people with AMD
- Severity: Wet AMD typically causes more severe vision loss despite being less common
- Symptoms: Both types can cause central vision problems, but wet AMD often produces more dramatic symptoms like sudden distortion or dark spots
- Underlying cause: Dry AMD involves drusen deposits and gradual cell breakdown, while wet AMD results from abnormal blood vessel growth and leakage
- Treatment options: Dry AMD has limited treatment options focused on lifestyle changes and supplements, while wet AMD has several medical interventions available
How Is AMD Diagnosed?
Your eye doctor can use several methods to diagnose AMD and determine which type you have. A comprehensive eye exam typically includes:
- Visual acuity test
- Dilated eye exam
- Amsler grid test
- Optical coherence tomography (OCT)
- Fluorescein angiography
Treatment Options for AMD
Treatment approaches differ significantly between dry and wet AMD, reflecting the distinct nature of each condition.
Dry AMD Treatments
Currently, no medical treatments can reverse dry AMD, but several strategies can help slow its progression:
- AREDS2 supplements: This specific combination of vitamins and minerals can slow the progression of AMD. These supplements typically contain vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin
- Lifestyle modifications: Maintaining a healthy diet rich in leafy greens, exercising regularly, not smoking, and protecting your eyes from UV light can all help slow AMD progression
- Low Vision: Low vision aids and magnifying devices, computer programs, and new emerging AI technology.
Wet AMD Treatments
Wet AMD offers more active treatment options, though early intervention is crucial for the best outcomes:
- Anti-VEGF Injections: These medications, injected directly into the eye, block the protein that causes abnormal blood vessel growth
- Photodynamic therapy: This treatment combines light-sensitive medication with laser therapy to destroy abnormal blood vessels
- Laser surgery: In some cases, direct laser treatment can seal leaking blood vessels, though this approach is less commonly used today
Take Steps to Protect Your Vision
Understanding the differences between wet and dry AMD empowers you to make informed decisions about your eye health. While both types of AMD can impact your vision, early detection and appropriate management can help preserve your sight and quality of life.
Regular eye exams remain your best defence against AMD, especially if you’re over 50 or have risk factors like family history or smoking. If you’ve been diagnosed with either type of AMD, work closely with your optometrist and follow their recommendations to help slow progression and maintain your independence.
If you’re experiencing any symptoms discussed above or it’s been a while since your last exam, contact your eyecare provider to book an appointment.